BNP (B-type natriuretic peptide) is a cardiac neurohormone secreted from cardiac ventricular myocyte in response to increased ventricular wall stretch or wall tension, increased ventricular volume or pressure. It is a potent vasodilator and it promotes diuresis. The half-live is short, about 18-22 minutes.
- Circulating BNP level increases in proportion to the severity of heart failure.
- Conditions
that raise BNP level beside heart failure
- Age, sex (female), left ventricular hypertrophy, acute coronary syndrome, acute myocardial infarction, cardiac inflammation, arrhythmogenic RV with decrease ejection, primary pulmonary hypertension, worsening of corpulmonale with increased RV pressure and volume, acute pulmonary emboli, Kawasaki disease, advanced renal failure, cirrhosis, hyperaldosteronism, Cushing syndrome, and decreased clearance.
- Heart
failure conditions that may have low BNP
- Flash pulmonary edema within 1 hour, acute chordal rupture, pulmonary congestion-edema from mitral stenosis, severe end stage heart failure, and heart failure in obese patients (BMI>30 kg/m2).
Potential usefulness are:
1. Diagnosis for HF
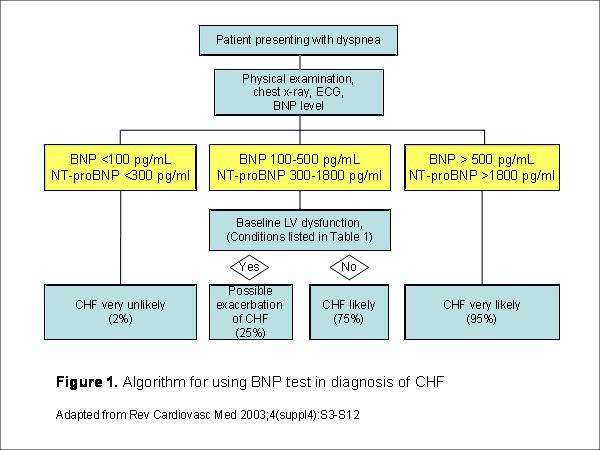
- Utilization
of BNP level to help differentiate heart failure from other causes of dyspnea
in ER or urgent care setting, using Point of Care measurement technique. BNP level
over 100 pg/ml favors the diagnosis of heart failure. The range of BNP level in
most heart failure patients is from a few hundreds to >1000 pg/ml. BNP
should not be a stand alone test. Clinical judgment is always important, Elevated
BNP are seen in other conditions (Table 1). Low BNP may be found in few acute
heart failure conditions and in obese patients with heart failure.
Table 1. Common causes of BNP elevation in routine clinical practice
Age. Female
Renal failure (Cr >2) or on dialysis
Myocardial infarction
Acute coronary syndromePulmonary disease with right-side failure
Acute pulmonary embolism
Sepsis
Baseline left ventricular dysfunction
- Utilization of BNP level as a diagnostic tool for heart failure with preserved systolic function. A heart failure patient with normal echocardiographic LV systolic function, abnormal diastolic filling abnormalities and elevated BNP should favor this diagnosis.
2. Follow up and Prognosis of heart failure
- During inpatient treatment of heart failure. Rising of the discharged BNP level from the admission level is a good predictor of poor prognosis and near future unfavorable outcome i.e... early readmission.
- During outpatient treatment followup, BNP guiding intensity of treatment may be useful.
- During acute MI, rising of BNP level few days after admission level indicates poorer prognosis.
- Baseline BNP is necessary for comparison
3. Treatment for acute decompensation
- Nesiritide (Natrecor) is a human recombinant BNP.
- Dosage: Intravenous 2 microgram/kg bolus, followed by infusion of 0.01 microgram/kg/min.
- Duration: Up to 7 days (or more?).
- Action: Hemodynamic effect is observed in an hour or less. There is no tolerance for several days of infusion. Hemodynamic effect resolves by 2-4 hours after cessation of the infusion.
- Nesiritide promotes diuresis.
- Use appropriate dose of diuretic. Over diuresing may potentiate hypotension side effect.
- Side effects: Hypotension (more in cases taking ACEI), nausea, headache.
- Caution: Volume depletion, aortic stenosis, hypertrophic cardiomyopathy, cardiogenic shock.
- Usually does not require hemodynamic monitoring.
- Beware of drug incompatibility in the infusion process.
- May obtain proBNP but not BNP level during nesiritide infusion.
- In the responder cases, if the BNP level is checked 2 hours (or more) after stopping the infusion it should be lower than the preinfusion level.
4. Potential outpatient intermittent treatment in severe heart failure
(Waiting for FUSION 2 trial)
5.NT-proBNP (NT = N Terminal)
When cardiac myocyte Pro-BNP enter the circulation it split into BNP which is an active neurohormone and NT-proBNP which is inactive part but with longer half life. Level of NT-proBNP can be used for diagnosis, follow up and prognosis of heart failure the same way as BNP level. The physicians need to know whether the report are BNP or NT-proBNP since the level are significantly different and some laboratory may not label it correctly.