-
Dub Sukhum, MD.
Warfarin Tablet
| (2009 update) |
Chapter 1
- Warfarin characteristic.
- Average Warfarin daily dose.
- Factors effect the Warfarin daily dose.
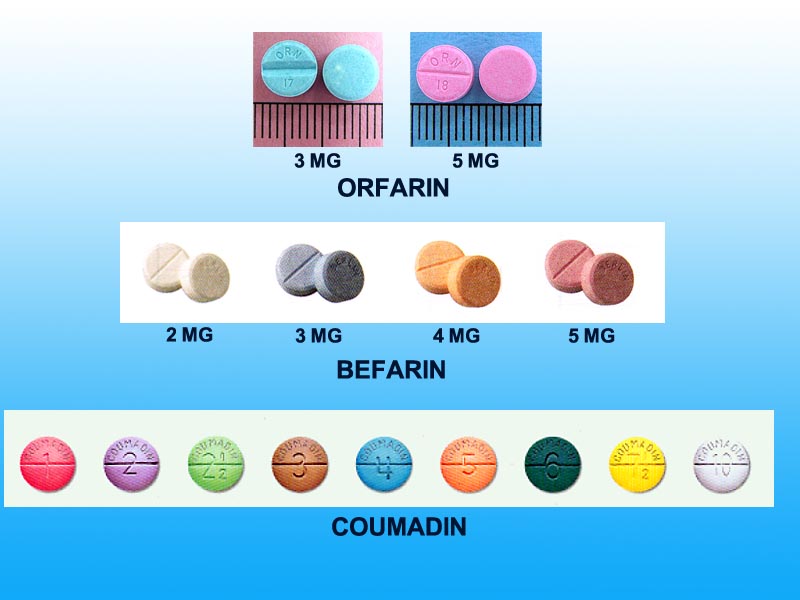
- Warfarin tablets
- Generic Warfarin (More update)
- Treatment Monitoring, standard and Point of Care
Chapter 2
- Initiation dose.
- Inpatient.
- Outpatient.
- Ethnic Difference for Pacific-Asian or Chinese-Asian
- Table. Warfarin Initiation
- Maintenance dose.
- Weekly dose.
- Daily schedule.
- Dose adjustment
- Warfarin dose schedule table.
Chapter 3
- Target INR.
- Target INR for Atrial Fibrillation-Atrial Flutter
- Target INR for Venous Thrombosis (DVT and PE)
- Target INR for Various Conditions
- Target INR for Heart Valve Prostheses
Chapter 4
Chapter 5
Chapter 6
Drugs interact with warfarin (Updating)
Chapter 7
References and anticoagulation web sites. (Updating)
Chapter 8
Patient Warfarin Booklet (Thai)
Patient Warfarin Personal Book (Thai)
This guideline was prepared for outpatient Warfarin (Coumadin) management, related to cardiology work such as atrial fibrillation and prosthetic heart valve. Other conditions are briefly included.
This guidelines was first prepared in 2001, for Central Minnesota Heart Center Anticoagulation Clinic. There was an 2004 updated. In 2007 this guidelines has inserted ethnic difference information in few appropriate areas, to be the guidelines for Bangkok Hospital Anticoagulation Clinic program. It follows the major anticoagulation guidelines, i.e. 8th ACCP Consensus Conference on Antithrombotic Therapy (Chest 2008), ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation and ACC/AHA 2006 practice Guidelines for the Management of Patients with Valvular Heart Disease. Some other databases are also listed in the bibliography section. Database on ethnic difference is limited at the present time.
It is expected that physicians may choose different approaches in certain patients for various reasons, however uniform practice will make the anticoagulation clinic run more efficiently.
There are differences among various ethnic
About 4-5 mg/day or 28-35 mg/week for caucasian for target INR of 2.5 (2.0-3.0)
About 3-4 mg/day or 21-28 mg/week for Pacific-Asian (exclude caucasian in this region). This dose will be less if INR level is recommended at <2.0.
Warfarin tablets ( Click here to view warfarin tablets)
Generic. When use generic warfarin, only one generic brand should be prescribed for each patient and it should be indicated that brand in the prescription.
Standard
Traditionally patients come into the clinic (or the hospital) to have venous blood drawn for routine laboratory INR determination.
Point of Care
Finger tip capillary blood can be used with small, light weight and portable instruments. The clinical trials result have compared favorably with traditional INR determination.
Use in anticoagulation clinic.
- Need good quality control for point of care INR measurement.
- Faster INR result. Patients are more willing to wait for the result before they go home.
- Direct patient contact for instruction before the patients leave the clinic is more efficient than phone call for the result later.
Home use or Patient Self Test (PST)
- Need good quality control for point of care INR measurement.
- Patient selection is essential.
- Patients must have long term indication for anticoagulation therapy..
- Patients must be willing and able to perform self-management.
- Patients must be willing to record results accurately and attend clinics regularly for quality assurance.
- Patients must demonstrate competence in using the instrument and interpreting the results.
- Patients must not have shown previous noncompliance in terms of clinic attendance or medication management.
- Can increase INR testing frequency and decrease complications associated with oral anticoagulation therapy.
Point of Care Instruments
Instrument Company Sample Type CoaguChek Roche Diagnostics Corp. Indianapolis, IN
http://www.coaguchek.com/landing/Capillary or venous whole blood Harmony INR Monitoring System LifeScan Inc., Milpitas, CA
www.lifescan.comCapillary or venous whole blood INRatio Prothrombin Time Monitoring System Hemosense, Inc. Milpitas, CA
www.hemosense.comCapillary or venous whole blood ProTime Microcoagulation System International Technidyne Corp. Edison, NJ
www.itcmed.comCapillary or venous whole blood
- These instruments are FDA approved for home use.
- These instruments are small, light weight, and portable devices.
Day 1
(If there is an active or acute thromboembolic condition, warfarin should be started along with heparin, unless there is a contraindication or patient cannot take medicine orally. Following warfarin initiation, heparin should be continued until INR reaches therapeutic level for 2 days).
5 mg (2.5-7.5). This dose is a good choice since it is known that average daily dose is close to 5 mg. Rapid increase INR (anticoagulant) will not achieve fast full antithrombotic effect since factor II half-life is up to 72 hours. Using higher dose than necessary may lead to bleeding complication due to rapidly and severely reduce factor VII. It may deplete protein C too quick, and theoretically can cause hypercoagulable state. The 5 mg size tablet is recommended for both inpatient and outpatient use, making inpatient to outpatient transition more convenient. It is the most commonly used size tablet by the majority of anticoagulation clinics today. If the dose should be changed, it can be given 0.0, 2.5, 5.0, 7.5, 10.0,---- with this size tablet.
The higher dose warfarin initiation have also been tested successfully by using normogram. It may be considered in patient who may need shorter period of time to reach therapeutic INR. It should be done in patient not in the list of "Lower dose" below. INR have to be done frequently enough to prevent over anticoagulation and bleeding complication
Lower dose (2.5 mg).Higher dose (7.5-10.0 mg).
- >80 yr.
- Concurrent illness.
- On interaction drug.
- S/P major surgery, i.e.. heart valve surgery.
- Chronic malnourished.
- Impaired liver function, liver congestion.
- Young healthy subject.
- In the first two days.
Day 2
A. If INR <1.5, continue the same dose.
B. If INR >1.5, give lower dose (2.5 mg or none)Day 3
For #A. of Day 2For #B. of Day 2
- If INR <1.5, suggests a higher than average maintenance dose of 5 mg/day or 35 mg/week will be needed. Give higher dose than 5 mg. i.e.7.5 mg for now.
- If INR 1.5-2.0, suggests an average maintenance dose close to 5 mg/day or close to 35 mg/week will be needed, and continue 5 mg for now.
- If INR >2.0, suggests a lower than average maintenance dose of 5 mg/day or 35 mg/week will be needed. Give less than 5 mg, i.e.2.5 mg or none for now.
- If INR 1.5-2.0, suggests daily dose will be close to or less than 5 mg/day or close to 35 mg/week or less. May give 5 mg or less for now.
- If INR >2.0, suggests daily dose will be lower than 5 mg/day or less than 35 mg/week. May give 2.5 mg or none for now.
Day 4
If there is no need for heparin therapy, the patient may have been discharged by now, and warfarin initiation is continued as an outpatient.
- INR 2 times a week until INR is in target range twice in a row, then INR 1 time weekly until INR is in target range twice in a row, then INR 1 time in 2 week until INR is in target range twice in a row, then enter the patient in to maintenance schedule (usually INR every 4 weeks).
- Patients during an acute illness, or post operative of major surgeries may be more sensitive to warfarin than when they become more stable.
Frequent INR measurement during warfarin initiation will help:
1. Reaching target INR in shorter period of time
2. Prevent bleeding complication from over anticoagulation
Out patient (See also "Day 4" above)
Table. Warfarin Initiation (for patient with average daily dose of 5 mg and target INR >2.0)
|
DAY |
INR |
DOSE |
|
| INPATIENT (Usually with daily INR) |
OUTPATIENT | ||
| 1 |
Normal |
5.0
mg ( 2.5 or 7.5-10.0 mg in patients listed in the text ) |
5.0
mg ( 2.5 or 7.5-10.0 mg in patients listed in the text ) |
| 2 |
< 1.5 |
5.0
mg 0.0 - 2.5 mg |
5.0
mg 0.0 - 2.5 mg |
| . | . | [If
INR is not measured 5.0 mg] |
|
| 3 |
< 1.5 1.5 - 1.9 2.0 - 3.0 > 3.0 |
5.0
- 10 mg 2.5 - 5.0 mg 0.0 - 2.5 mg 0.0 mg |
5.0
- 10 mg 2.5 - 5.0 mg 0.0 - 2.5 mg 0.0 mg |
. |
. |
INR should be measured today. If INR is not measured, may use the same dose as day 2, and should not > 5 mg | |
| 4 |
<1.5 1.5 - 1.9 2.0 - 3.0 > 3.0 |
10.0
mg 5.0 - 7.5 mg 0.0 - 5.0 mg 0.0 mg |
10.0
mg 5.0 - 7.5 mg 0.0 - 5.0 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 3 is <1.5 or >3.0 | |
| 5 |
< 1.5 1.5 - 1.9 2.0 - 3.0 > 3.0 |
10.0
- mg 7.5 - 10.0 mg 0.0 - 5.0 mg 0.0 mg |
10.0
- mg 7.5 - 10.0 mg 0.0 - 5.0 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 4 is <1.5 or >3.0 | |
| 6 |
< 1.5 1.5 - 1.9 2.0 - 3.0 > 3.0 |
7.5
- 12.5 mg 5.0 - 10.0 mg 0.0 - 7.5 mg 0.0 mg |
7.5
- 12.5 mg 5.0 - 10.0 mg 0.0 - 7.5 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 5 is <1.5 or >3.0 | |
Note: Frequent INR measurement during warfarin initiation helps prevent bleeding from over anticoagulation and helps reaching target INR sooner. |
|||
Table. Warfarin Initiation (for patient with average daily dose of 3 mg and target INR >1.6)
|
DAY |
INR |
DOSE |
|
| INPATIENT (Usually with daily INR) |
OUTPATIENT | ||
|
1 |
Normal |
3.0 mg ( 1.5 or 3.0-6.0 mg in patients listed in the text ) |
3.0 mg ( 1.5 or 3.0-6.0 mg in patients listed in the text ) |
|
2 |
< 1.3 |
3.0 mg 0.0 - 1.5 mg |
3.0 mg 0.0 - 1.5 mg |
| . | . | [If INR is not measured 3.0 mg (1.5-4.5)] |
|
|
3 |
< 1.3 1.3 - 1.6 1.6 - 2.6 > 2.6 |
3.0 - 6 mg 1.5 - 3.0 mg 0.0 - 1.5 mg 0.0 mg |
3.0 - 6 mg 1.5 - 3.0 mg 0.0 - 1.5 mg 0.0 mg |
. |
. |
INR should be measured today. If INR is not measured, may use the same dose as day 2, and should not > 3.0 mg | |
|
4 |
<1.3 1.3 - 1.6 1.6 - 2.6 > 2.6 |
4.5 - 6.0 mg 3.0 - 4.5 mg 1.5 - 3.0 mg 0.0 mg |
4.5 - 6.0 mg 3.0 - 4.5 mg 0.0 - 3.0 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 3 is <1.3 or >2.6 | |
|
5 |
< 1.3 1.3 - 1.6 1.6 - 2.6 > 2.6 |
6.0 - 7.5 mg 3.0 - 4.5 mg 1.5 - 3.0 mg 0.0 mg |
6.0 - 7.5 mg 3.0 - 4.5 mg 1.5 - 3.0 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 4 is <1.3 or >2.6 | |
|
6 |
< 1.3 1.3 - 1.6 1.6 - 2.6 > 2.6 |
6.0 - 7.5 mg 4.5 - 6.0 mg 1.5 - 3.0 mg 0.0 mg |
6.0 - 7.5 mg 4.5 - 6.0 mg 1.5 - 3.0 mg 0.0 mg |
| . | . | INR measurement should be done, if INR on day 5 is <1.3 or >2.6 | |
Note: Frequent INR measurement during warfarin initiation helps prevent bleeding from over anticoagulation and helps reaching target INR sooner. |
|||
(Example for patient with average daily dose of 5 mg)
Back ground
- Because warfarin has a long half-life and there is a range for INR (i.e. 2.0-3.0) to work with, there is no need to keep an equal daily dose. In fact it is impossible to do that, since the patient will have to use several tablet size to fit to the different daily dose requirement during the long term follow up. This will create confusion.
- Using specific days of the week for different daily dose is less confusing.
- There is no significant INR swing as long as the daily dose difference is not large (i.e. <2.5 mg, when use 5 mg size tablet).
- Using weekly dose adjustment appears more convenient and it is just as accurate.
- Applying the above principle along with one size tablet (i.e. 5 mg or 3 mg), a table of weekly-daily dose schedule can be constructed for working convenience (see Warfarin dose schedule table for 5 mg tablet and 3 mg tablet)
- Note that weekly dose difference can be arranged as low as 2.5 mg per week, equivalent to only 0.4 mg per day difference.
Example
Weekly Dose (mg)/ Daily Dose (mg)
- 35 -------------- 5.0 daily
- 37.5 ----------- 7.5 Mon, 5 ROW
- 40 -------------- 7.5 Mon, Fri, 5 ROW
- 42.5 ----------- 7.5 Mon, Wed, Fri, 5 ROW
- 45 -------------- 5.0 Mon, Wed, Fri, 7.5 ROW
- 47.5 ------------ 5.0 Mon, Fri, 7.5 ROW
- -------------------------
(ROW = Rest Of the Week)
Weekly Dose Mon Tue Wed Thu Fri Sat Sun 35 5 5 5 5 5 5 5 37.5 7.5 5 5 5 5 5 5 40 7.5 5 5 5 7.5 5 5 42.5 7.5 5 7.5 5 7.5 5 5 45 5.0 7.5 5.0 7.5 5.0 7.5 7.5 47.5 5.0 7.5 7.5 7.5 5.0 7.5 7.5
Note: Patient should take warfarin in PM (i.e.5-7 PM), and have INR test in AM, for consistency of the INR result. This also allows time to contact the patient before the patient takes warfarin that day.
Table 1. Warfarin Dose Schedule for 5 mg Tablet (2 mg when eekly dose is < 15 mg)
ROW ROW ROW ROW ROW Daily ROW ROW ROW ROW ROW ROW Daily . . . . . ROW ROW ROW Daily ROW ROW ROW ROW ROW ROW Daily ROW ROW ROW ROW . . . . . . ROW ROW
- All doses are in mg.
- M,W,and F - Monday, Wednesday and Friday
- ROW - Rest Of the Week
Table 1. Warfarin Dose Schedule for 3 mg Tablet (2 mg when weekly dose is < 18 mg)
2 1.0 ROW 2 31.5 . . 3 3 1.0 0.0 ROW 2 33 6.0 4.5 3 4 0.0 1.0 ROW 2 34.5 6.0 4.5 3 5 0.0 1.0 ROW 2 36 6.0 4.5 3 6 0.0 1.0 ROW 2 37.5 4.5 6.0 3 7 . . 1.0 Daily 2 39 4.5 6.0 3 8 2.0 1.0 ROW 2 40.5 4.5 6.0 3 9 2.0 1.0 ROW 2 42 . 6.0 3 10 2.0 1.0 ROW 2 43.5 7.5 6.0 3 11 1.0 2.0 ROW 2 45 7.5 6.0 3 12 1.0 2.0 ROW 2 46.5 7.5 6.0 3 13 1.0 2.0 ROW 2 48 6.0 7.5 3 14 . 2.0 Daily 2 49.5 6.0 7.5 3 15 3.0 2.0 ROW 2 51 6.0 7.5 3 16 3.0 2.0 ROW 2 52.5 . 7.5 3 17 3.0 2.0 ROW 2 54 9.0 7.5 3 18 2.0 3.0 Daily 2 55.5 9.0 7.5 3 . . . . . 57 9.0 7.5 3 13.5 3.0 1.5 ROW 3 58.5 7.5 9.0 3 15 3.0 1.5 ROW 3 60 7.5 9.0 3 16.5 1,5 3.0 ROW 3 61.5 7.5 9.0 3 18 1.5 3.0 ROW 3 63 . 9.0 3 19.5 1.5 3.0 ROW 3 64.5 10.5 9.0 3 21 . 3.0 Daily 3 66 10.5 9.0 3 22.5 4.5 3.0 ROW 3 67.5 10.5 9.0 3 24 4.5 3.0 ROW 3 69 9.0 10.5 3 25.5 4.5 3.0 ROW 3 70.5 9.0 10.5 3 27 3.0 4.5 ROW 3 . . . . . 28.5 3.0 4.5 ROW 3 ROW 3
- All doses are in mg.
- M,W,and F - Monday, Wednesday and Friday
- ROW - Rest Of the Week
To change the warfarin weekly dose:
a) Change warfarin weekly dose by 10% (5-15%). Use higher percentage in patients with higher warfarin weekly dose,
b) The new Warfarin dose should not be significantly different from many recent adequate doses on patient record.
c) Repeat INR in 1-2 weeks.
With the same diagnosis, co-morbidity or risk factors may move target INR to the higher level or add low dose ASA (75-325 mg), i.e. bileaflet aortic valve prostheses with recurrent systemic emboli should add ASA 75-325 mg and/or move up target INR from 2.0-3.0 to 2.5-3.5. Remember that INR >4.0 is associated with significant more bleeding.
Target INR for various conditions
This guidelines will offer few approaches based on the published major guidelines. The reader may select any of these approaches.
Adapt From ANTITHROMBOTIC AND THROMBOLYTIC THERAPY, 8TH ED: ACCP GUIDELINES : Executive Summary
Table 2. Target INR for Atrial Fibrillation and Atrial Flutter.
. ATRIAL FIBRILLATION A fib, < 75 yr. without RF1 and RF2
A fib, with any one of RF2
A fib, with two or more of RF2
A fib, with RF1
A fib, with recurrent emboli.
A fib, following cardiac surgery †
2.0-3.0 †† . . A fib, <48 hr
. A fib. Pre-cardioversion (>48 hr)
.
Post-cardioversion (>48 hr)
.I Long-term ** .
ATRIAL FLUTTER. For Pacific-Asian (exclude caucasian in this region), The INR range of 2.0-3.0 and 2.5-3.5 may be substituted with INR range of 1.6-2.6 and 2.0-3.0 respectively (Requires more validation)
- RF1 = Risk Factors1: History of ischemic stroke or systemic emboli.
- RF2 = Risk Factors2: (1). Age >75 yr, (2). Hypertension. (3). Diabetes Mellitus. (4). CHF/moderate to severe impaired LV systolic function.
- a = add ASA 75-325 mg when there are more risk factors or more emboli.
- † = If >48 hours.
- †† = The anticoagulation treatment should continue for several weeks following reversion to NSR, particularly if patients have risk factors for thromboembolism. There is no need for long term anticoagulation if atrial fibrillation occurs only post operatively and revert or convert to NSR.
- ** = Base from "Rate vs Rhythm Control" trials, patients should be on long term anticoagulation if they have higher risk factors
ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation
Circulation. 2006;114:e257-e354.The 2006 ACC/AHA/ESC guidelines emphasized on risk/benefit of thromboembolism and major bleeding for anticoagulation decision. There are 3 options.
Option 1: Using low, medium and high risk factors for thromboembolic score
Antithrombotic Therapy for Patient With Atrial Fibrillation
No risk factors Aspirin 81-325 mg daily One moderate-risk factor Aspirin 81-325 mg daily, or
Warfarin (INR 2.0-3.0), target 2.5Any high-risk factor,
More than one moderate-risk factorWarfarin (INR 2.0-3.0), target 2.5
Female gender,
Age 65-74 y,
Coronary artery disease,
ThyrotoxicosisAge >75 y,
Hypertension,
Heart failure,
LVEF <35%,
Diabetes mellitusPrevious stroke, TIA,
Systemic embolism
Mitral stenosis,
Prosthetic heart valve** If mechanical valve, target INR >2.5
Option 2 : Using CHADS2 Index
Stroke Risk in Patients With Nonvalvular AF Not Treated With Anticoagulation According to the CHADS2, IndexThere are several stroke risk scores available and CHADS2 index is a simple and reasonable accurate for clinical use. Warfarin should be prescribed for the patient with CHADS2 score of 2 or higher.
CHADS2, Risk Criteria Score Prior stroke or TIA
Age >75 y
Hypertension
Diabetes mellitus
Heart failure2
1
1
1
1
(N=1723)
(95% CI)
(INR 2.0-3.0 )
463
523
337
220
65
5
2.8 (2.0 to 3.8)
4.0 (3.1 to 5.1)
5.9 (4.6 to 7.3)
8.5 (6.3 to 11.1)
12.5 (8.2 to 17.5)
18.2 (10.5 to 27.4)
1
2
3
4
5
6.
.
Yes
Yes
Yes
Yes
YesOption 3:
2006 ACC/AHA/ESC Risk-Based Approach to Antithrombotic Therapy in Patients With Atrial Fibrillation
<60 yr. No heart disease ( lone AF) ASA 81-325 mg/day
or no therapy<60 yr with heart disease. No RF* ASA 81-325 mg/day 60-74 yr. No RF* ASA 81-325 mg/day 65-74 yr with DM or CAD Warfarin (INR 2.0-3.0) >75 yr. Women Warfarin (INR 2.0-3.0) >75 yr. Men. No RF* Warfarin (INR 2.0-3.0)
or ASA 81-325 mg/day>65 yr and heart failure Warfarin (INR 2.0-3.0) LV ejection fraction <35% and HT Warfarin (INR 2.0-3.0) Rheumatic heart disease (MS) Warfarin (INR 2.0-3.0) Prosthetic heart valves Warfarin (INR 2.0-3.0 or higher) Prior thromboembolism Warfarin (INR 2.0-3.0 or higher) Persistent atrial thrombus on TEE Warfarin (INR 2.0-3.0 or higher) AF = Atrial fibrillation. MS = Mitral stenosis. DM = Diabetes mellitus. HT = Hypertension
RF* = Risk factors for thromboembolism: Heart failure (HF), LVEF < 35, and HTFor Pacific-Asian (exclude caucasian in this region), The INR range of 2.0-3.0 and 2.5-3.5 may be substituted with INR range of 1.6-2.6 and 2.0-3.0 respectively (Requires more validation)
Table 3. Target INR for Venous Thromboembolism. Deep Vein Thrombosis (DVT) and Pulmonary Emboli (PE)
Adapt From ANTITHROMBOTIC AND THROMBOLYTIC THERAPY, 8TH ED: ACCP GUIDELINES : Executive Summary
Secondary (reversable cause) deep vein thrombosis (DVT) or pulmonary emboli (PE). First episode
. Idiopathic DVT or PE. First episode
2.0-3.0
6-12 monthsMay consider long-term, particularly proximal DVT Idiopathic DVT or PE. Second episode
Long-term3 months for distal DVT DVT or PE with cancer
Until cancer is resolvedLMWH for the first 3-6 months DVT or PE with antiphospholipid antibodies. First episode
12 monthsMay consider long- term DVT or PE with deficiency of coagulation factors *. First episode
6-12 monthsRecurrent episodes of DVT or PE
Long-term. For Pacific-Asian (exclude caucasian in this region), The INR range of 2.0-3.0 and 2.5-3.5 may be substituted with INR range of 1.6-2.6 and 2.0-3.0 respectively (Requires more validation)
- Start heparin with warfarin. Prefer Low molecular weight heparin (LMWH) over Unfractionated heparin (UFH).
- Discontinue heparin 2 days after target INR has reached.
- May use thrombolytic treatment in massive or life threatening pulmonary emboli.
- Duration of 12 months or more in cases of recurrent VTE, cancer, antithrombin deficiency, antithrombin antibody syndrome, protein C or protein S deficiency,
- * = multiple thrombophilic conditions, antithrombin deficiency, antithrombin antibody syndrome, protein C or protein S deficiency, hemocystienemia, homozygous factor V Leidin.
- Insert inferior vena caval filter in cases of high risk of VTE and cannot use anticoagulation, recurrent VTE or pulmonary emboli with pulmonary hypertension despite adequate anticoagulation.
Table 4. Target INR for various conditions
Adapt From ANTITHROMBOTIC AND THROMBOLYTIC THERAPY, 8TH ED: ACCP GUIDELINES : Executive Summary
. LEFT VENTRICULAR DISEASE . Dilated cardiomyopathy (EF<30%).
Dilated cardiomyopathy (EF<30%), & emboli.
S/P anterior MI, LV thrombus.
SYSTEMIC EMBOLI. Systemic emboli.
. VALVULAR DISEASES. Rheumatic MV disease, NSR, LA > 5.5 cm,
Mitral valvuloplasty 2.0-3.0 3 wk before,
4 wk after. ( MV prolapse, unexplained TIA or ischemic stroke
.ASA 50-100
Mitral annular calcification (MAC).
MAC, systemic emboli (calcific) without atrial fibrillation
.ASA 50-100
AV disease
(No anticoag. Rx by itself) . . . . PFO OR ATRIAL SEPTAL ANEURYSM. PFO with ischemic stroke
ASA 50-100
. PFO with cryptogenic ischemic stroke particular with DVT
PFO. ENDOCARDITIS. Native valve or bioprotheses, with systemic emboli during endocarditis.
Mechanical prostheses, during endocarditis. . . Nonbacterial thrombotic endocarditis (NBTE) with systemic or pulmonary emboli.
Aseptic vegetation (in patients with disseminated cancer or debilitating disease)
. . . . ASCENDING AORTA, AORTIC ARCH. Ascending aorta, aortic arch. Mobile plaque >4 mm (TEE).
For Pacific-Asian (exclude caucasian in this region), The INR range of 2.0-3.0 and 2.5-3.5 may be substituted with INR range of 1.6-2.6 and 2.0-3.0 respectively (Requires more validation)
- a = add ASA 50-100 mg when there are more risk factors or more emboli. Use Dipyridamole 400 mg/d or clopidogrel 75 mg/d if the patients can not take ASA.
- Note that the lowest ASA dose in this table is 50 mg. The recommended lowest ASA dose in atherosclerotic disease is 75 mg.
Target INR for Heart Valve Prostheses
General principles
- Type of prostheses. St. Jude Medical bileaflet, CarboMedics bileaflet, Medtronic-Hall tilting mono disc, Omnicarbon mono tilting disc, and Sorin bileaflet, in aortic position, are less thrombogenic. Mitral position is more thrombogenic than aortic position. First few days up to first few months after surgery is more thrombogenic. Multiple prostheses have higher thromboembolic risk than single prosthesis.
- High thromboembolic risk cases.
- Tilting disk, ball-caged, disk-caged (except Medtronic-Hall in aortic position).
- Risk factors (RF). Atrial fibrillation, severe LV systolic dysfunction, previous thromboembolism, hypercoagulable conditions.
- Continue thromboembolic problem while on treatment.
- Treatment.
- Add ASA (50)80-160 mg (up to 325).
- Increase the INR target level, i.e.2.0-3.0 to 2.5-3.5, up to 3.0-4.5. The latter is associate with higher bleeding complication.
Table 5. Target INR for Heart Valve Prostheses
Adapt From ANTITHROMBOTIC AND THROMBOLYTIC THERAPY, 8TH ED: ACCP GUIDELINES : Executive Summary
and ACC/AHA Pocket Guidelines. Management of Patients with Valvular Heart Disease, 2006.
GENERAL APPROACH * Mechanical prostheses(1)
May add ASA 50-100 Mechanical prostheses, others
May add ASA 50-100 Mechanical prostheses(3) Add ASA 50-100 Mechanical prostheses, with RF(2)
Add ASA 50-100 . AORTIC VALVE * AV prostheses, bileaflet (1), no RF(2)
May add ASA 50-100 AV prostheses, bileaflet (1), with RF(2)
Add ASA 50-100 AV prostheses, others, no RF(2)
May add ASA 50-100 AV prostheses, others, with RF(2)
Add ASA 50-100 AV bioprostheses, 1st 3 months
. -- After 3 months
. -- After 3 months, with RF(2)
May add ASA 50-100 . MITRAL VALVE * MV prostheses, mechanical
May add ASA 50-100 . MV bioprostheses, 1st 3 months
May add ASA 50-100 -- After 3 months
May add ASA 50-100 -- After 3 months, with RF(2)
May add ASA 50-100 For Pacific-Asian (exclude caucasian in this region), The INR range of 2.0-3.0 and 2.5-3.5 may be substituted with INR range of 1.6-2.6 and 2.0-3.0 respectively (Requires more validation)
- * = Warfarin can be started the day after prosthetic valve replacement. UFH or LMWH should be started about 2 days post surgery (when surgical bleeding has been completely controlled) and continue until INR reaches therapeutic level for 2 consecutive days.
- (1) = In aortic position.: St. Jude Medical bileaflet, CarboMedics bileaflet, Medtronic-Hall tilting mono disc, Omnicarbon mono tilting disc, and Sorin bileaflet.
- (2) = Risk factors: History of TIAs, CVA, systemic emboli, severe LV systolic dysfunction, recurrent CHF.
- Adding ASA is not recommended in patient with high risk bleeding.
- ASA dose: ACCP 8th Guidelines = 50-100 mg, ACC/AHA Pocket Guidelines = 75-100 mg
General principle
- Check for bleeding history.
- Treat patients with active or recent bleeding, history of easy bleeding or higher INR more aggressive.
- Require admission if there is significant bleeding.
- Hold warfarin until INR returns to therapeutic range or as long as there is bleeding or potential bleeding.
- Check INR more often during the period of higher INR or bleeding.
- Check for factor(s) effecting warfarin response. Try to correct it, or change dose appropriately.
- Individualization is necessary.
- INR > therapeutic level, but < 5.0 and no bleeding.
- Hold warfarin for 1-2 days. Check INR in 1-2 days. Restart warfarin when INR return to target level. Check for factor(s) effecting high INR before changing the warfarin dose.
- May not require warfarin dose change if the factor(s) effecting high INR can be identified and corrected.
- INR 5-9, and no bleeding.
- Hold Warfarin, check INR in 1 day. Restart warfarin when INR return to target level. Check for factor(s) effecting INR carefully, correct the problem.
- More likely will require warfarin dose change.
- May prescribe small dose of oral vitamin K (1-2.5 mg)
- INR < 10, with minor bleeding or high risk for bleeding (i.e. recent surgery).
- Hold warfarin. Vitamin K, 1-2.5 mg orally. Check for INR in 12-24 hours.May repeat vitamin K in 24 hours. Check for factor(s) effecting INR carefully, correct the problem.
- Restart warfarin when at appropriate time. Adjust the dose.
- INR 10-20, and no bleeding.
- Hold warfarin. Vitamin K 2.5-5.0 mg orally. Check INR in 12-24 hours. If there is no admission, patient education is important. Check for factor(s) effecting INR carefully, correct the problem.
- Restart warfarin when INR return to target range. Adjust the dose.
- INR 10-20, with more then minor bleeding.
- Require admission.Hold warfarin. Vitamin K 5-10 mg slow IV infusion (not >1 mg/min), and/or FFP (15 ml/kg). Check INR in 6-12 hours or after FFP administration, repeat vitamin K and/or FFP as necessary. Check for factor(s) effecting INR carefully, correct the problem.
- Restart warfarin when INR return to target range and the bleeding has resolved. Adjust the dose.
- INR > 20, with bleeding tendency or bleeding.
- Require admission. Hold warfarin. Vitamin K 5-10 mg slow IV infusion (not >1 mg/min), and/or FFP (15 ml/kg). Check INR in 6-12 hours or after FFP administration, repeat vitamin K and/or FFP as necessary. Check for factor(s) effecting INR carefully, correct the problem.
- Restart warfarin when INR return to target range and the bleeding has resolved. Adjust the dose.
- Serious bleeding with therapeutic or elevated INR.
- Require admission.
- Follow guideline #5. Be careful when restarting warfarin.
- Patient who requires more rapid or urgent reversal before procedure/surgery.
- Hold warfarin. Vitamin K 5-10 mg slow IV infusion (not >1 mg/min), and/or FFP (15 ml/kg).
- Check INR in 6-12 hours or after FFP administration, repeat vitamin K and/or FFP as necessary.
(Large dose of intravenous administration may cause a period of warfarin resistance up to a week, when restarts it.)
- The tablet size is 5 mg (in US). The practical smallest dose is 2.5 mg. (Dose of 1.0 mg can be obtained by withdrawing the right amount of Warfarin from a 10 mg vial of injectable vitamin K, dilutes with juice then given orally). Oral route is effective. Subcutaneous route may have unpredictable and delayed response. Intramuscular route may cause hematoma at the injection site.
- Intravenous route, utilizes when
- Patient is unable to take oral medicine.
- Patient who may have impair absorption.
- Need rapid reversal of the INR.
- Slow rate of infusion, at <1 mg/min, may help decrease the severity of anaphylactic reaction.
- Large dose of intravenous administration may cause a period of warfarin resistance up to a week, when restarts it.
Table 8. Managing high INR or bleeding.
Hold ----- Adjust dose
• * or Vitamin K 2.5 mg po.
• FFP - Fresh Frozen Plasma.
• PCC - Prothrombin Complex Concentration
Problems
- Lack of good database.
- Most physicians use their own approaches which vary and is inconsistent. Some of these approaches have not been based on good principle, but rather a guessing or compromised one.
Guidelines.
- Assess the thromboembolic risk of the condition that requires the anticoagulation treatment.
- Assess the bleeding risk of the procedure/surgery that will be performed.
- Possibility of hypercoagulable state induced by the withdrawal of warfarin (rebound phenomenon) or the surgical milieu resulting in greater perioperative thromboembolic events than what would be predicted based on the annual thromboembolic rate during nonsurgical settings (Table 9).
- Post major operative venous thromboemboli are more common, while post operative arterial thromboemboli are rare.
- Permanent disability or death is substantially more common after arterial thromboembolism (70-75%) compare to following venous thromboembolism (4-10%). Permanent disability or death after postoperative major bleeding is lower, at about 1-6%.
- Individualization.
- Select the plan in the "Protocol for managing anticoagulation during procedures/surgeries (5 plans)", then follow the detail of that plan in the "Detail of the protocol for managing anticoagulation during procedures/surgeries (5 plans) "
- Using the protocol will make this management more uniform.
Protocol for managing anticoagulation during procedures/surgeries.
- 5 plans for different days of inadequate anticoagulation ranging from 0 to 7 days. These plans include:
(1) Continue warfarin;
(2) Hold warfarin, pre and post heparin;
(3) Hold warfarin, post heparin;
(4) Hold warfarin, pre heparin:
(5) Hold warfarin only.
Using low molecular weight heparin allows us to use this protocol out of the hospital both pre and post procedures/surgeries, if necessary.- Too early post operative full dose heparin is associated with more bleeding complication, while pre operative heparin rarely causes bleeding, if withheld it at appropriate time.
For more urgent surgery, please review Section Managing High INR or Bleeding, "8. Patient who requires more rapid or urgent INR reversal before procedure/surgery".
Bridging Therapy is the procedure involving temporary use of heparin when the warfarin is withheld.
Thromboembolic Risks
Table 9. Risk of thromboembolism on patients without anticoagulation therapy. (Not during withholding warfarin for procedure/surgery). (Adapted from Kearon C, Hirsh J. Management of Anticoagulation Before and After Elective Surgery. NEJM 1997; 336:1506-1511).
VENOUS . Acute VTE
. -- Month 0-1
1.3
-- Month 1-3
Recurrent VTE
ARTERIAL
Acute arterial embolism
-- Month 0-1
NVAF
NVAF and previous embolism
Mechanical heart valve
- VTE = Venous thromboembolism. NVAF = Non valvular atrial fibrillation. * = Average
- † = Varies with type, position, and multiple prostheses.
(Rate of thromboembolism may be higher following holding warfarin and during surgical procedures - "rebound phenomenon")
Patients with high risk for thromboembolism.
(1 year risk of arterial embolism > 10%, or 1 month risk of venous thromboembolism > 10 %)
- Known hypercoagulable state: Protein C, protein S and antithrombin III deficiency. Factor V Leiden and prothrombin gene mutation.
- Antiphospholipid antibody syndrome (APS), SLE with cardiolipin antibodies.
- Recurrent arterial or idiopathic venous thromboembolism events.
- Venous or arterial thromboembolism within the preceding 1-3 months.
- Rheumatic atrial fibrillation.
- Acute intracardiac thrombus visualized by echocardiogram.
- Atrial fibrillation plus mechanical heart valve in any position.
- Older mechanical valve model in mitral position.
- Recently placed mechanical valve (<3 months).
- Atrial fibrillation with history of cardioembolism.
Patients with intermediate risk for thromboembolism.
(1 year risk of arterial embolism of 5 to 10%, or 1 month risk of venous thromboembolism of 5 to 10 %)
- Recurrent CVA or TIAs without risk factors for cardiac embolism.
- Atrial fibrillation without history of cardiac embolism but with multiple risks for cardiac embolism (LV ejection <40%, diabetes, hypertension, nonrheumatic valvular heart disease, transmural myocardial infarction within preceding month)
- Venous thromboembolism 3-6 months.
Patients with low risk for thromboembolism.
(1 year risk of arterial embolism < 5%, or 1 month risk of venous thromboembolism < 2%%)
- Venous thromboembolism >6 months.
- Atrial fibrillation without multiple risks for cardiac embolism.
- Newer model prosthetic valve in aortic position >3 months.
Bleeding Risks
- Low risk.
High risk.
- Cutaneous: Local skin surgery, i.e. Mohs micrographic surgery, simple excisions, biopsy and repairs.
- Oral: Simple dental procedures, i.e. simple tooth extraction, dental hygiene, restorations, endodontics, prosthetics and periodontal therapy. (Some dentists give antifibrinolytic agents such as tranexamic acid or epsilon aminocaproic acid mouthwash to help control local breeding).
- Joint and soft tissue aspirations and injections.
- Minor podiatric procedures, i.e. nail avulsions and phenol matrixectomy.
- Opthalmic: Cataract extraction, trabeculectomy. The rate of retrobulbar hemorrhage, subconjunctival hemorrhage and mild hyphema increases slightly, but with good prognosis. Risk of bleeding in vitreoretinal, complex lid, and orbital surgical procedures has not been adequately studied.
- Gastroenterologic: diagnostic esophago-gastro-duodenoscopy (EGD) with or without biopsy, flexible sigmoidoscopy with or without biopsy, colonoscopy with or without biopsy, diagnostic endoscopic retrograde cholangio-pancreatography (ERCP) without sphincterotomy, biliary stent insertion without endoscopic sphincterotomy, endosonography (EUS) without fine needle aspiration, and push enteroscopy of the small bowel. (There is the possibility of poIypectomy with endoscopic examination particularly the colonoscopy. Preparing these cases as high bleeding risk may help prevent repeating the procedure.)
- Cutaneous: More complex procedures, i.e. hair transplantation, blepharoplasty, or facelifts.
- Oral: More complex procedures such as complicated extractions, gingival and alveolar surgeries.
- Opthalmic: Retinal surgery, complex lid and orbital surgery, patients who need retrobulbar anesthesia for ophthalmic procedures.
- Gastroenterologic: Colonoscopic and gastric polypectomy, laser ablation and coagulation, endoscopic sphincterotomy, and those procedures with the potential to produce bleeding inaccessible or uncontrollable by endoscopic means such as pneumatic or bougie dilation of benign or malignant strictures, percutaneous endoscopic gastrostomy, and EUS-guided fine needle aspiration.Intracavitory surgery:
- Intraabdominal surgeries, intrathoracic surgeries, intracranial surgeries,
- Neurosurgical procedures, neuraxial anesthesia and spinal puncture.
- Orthopedic.
- Genito-urinary: Transurethral resection of the prostate?
- Obstetric-gynecologic.
- Cardiac procedures. Pacemaker/ICD insertion have more bleeding potential than bleeding from cardiac catheterization site.
- Any procedures or surgeries that bleeding can not be controlled or stopped with simple intervention.
- Other major surgeries.
Table 10. Protocol for managing anticoagulation during procedures/surgeries (5 plans)
Continue warfarin Hold warfarin With Pre and Post procedure heparin
Hold warfarin With Post procedure heparin Hold warfarin With Pre procedure heparin Hold warfarin only
* = Minimal days
The section below is for population who require target INR >2.0 (Caucasian). It should be modified for population who require difference target INR.
Detail of protocols for managing anticoagulation during procedures/surgeries (Table 10)
- Plan 1: Continue warfarin.
- Check INR 7 days before the procedure, keep INR in low target range. Communicate with operator who will perform the procedure.
- This protocol will result in no subtherapeutic anticoagulation day.
- Plan 2: Hold warfarin, post procedure heparin, pre procedure heparin.
- Check INR 7 days before procedure, keep INR in target range.
- Drop INR to 1.5 or less. For INR of 2.0-3.0, it will require about 4(3-5) days. Higher INR will take longer time.
- Start full dose of unfractionated heparin (UFH) or low molecular weight heparin (LMWH) when INR is 2.0 or less which may take about 24-48 hours for INR of 2.0-3.0.
- Check INR 1 day before the procedure. If INR is 1.8 or higher, give vitamin K 2.5 mg orally, or delay the procedure.
- Stop heparin (6 hours for UFH, or 24 hours for LMWH) before the procedure.
- Start full dose of heparin (UFH or LMWH) 24 hours post procedure (when there is no risk of post operative bleeding). No bolus. (This full dose heparin using early postoperatively only apply in patients with low risk for post operative bleeding).
- Low dose (for venous thromboemboli prevention) may be started 12 hours post procedure.
- These post procedure heparin timing should be varied (delayed) depending on risk of bleeding for that patient.
- Restart the previous maintenance dose of warfarin the evening of the procedure. If it cannot be started - see "Remark" below.
- This protocol will result in subtherapeutic anticoagulation for 1-2 days.
- Plan 3: Hold warfarin, post procedure heparin. (Not suitable for patients with high risk for post procedures/surgeries bleeding)
- Check INR 7 days before the procedure, keep INR in target range.
- Drop INR to 1.5 or less. For INR of 2.0-3.0, it will require about 4(3-5) days. Higher INR will take longer time.
- Check INR 1 day before the procedure. If INR is 1.8 or higher, give vitamin K 2.5 mg orally, or delay the procedure.
- Start full dose of heparin (UFH or LMWH) 24 hours post procedure (when there is no risk of post operative bleeding). No bolus. (Only apply in patients with low risk for post operative bleeding).
- Low dose ( for venous thromboemboli prevention) may be started 12 hours post procedure.
- These post procedure heparin timing should be varied (delayed) depending on risk of bleeding for that patient.
- Restart the previous maintenance dose of warfarin the evening of the procedure. If it cannot be started - see "Remark" below.
- This protocol will result in subtherapeutic anticoagulation for 3-4 days.
- Plan 4: Hold warfarin, pre procedure heparin.
- Check INR 7 days before procedure, keep in target range.
- Drop INR to 1.5 or less. For INR of 2.0-3.0, it will require about 4(3-5) days. Higher INR will take longer time.
- Start full dose of unfractionated heparin (UFH) or low molecular weight heparin (LMWH) when INR is 2.0 or less which may take about 24-48 hours for INR of 2.0-3.0.
- Check INR 1 day before the procedure. If INR is 1.8 or higher, give vitamin K 2.5 mg orally, or delay the procedure.
- Stop heparin (6 hours for UFH, or 24 hours for LMWH) before the procedure.
- Restart the previous maintenance dose of warfarin the evening of the procedure. If it cannot be started - see "Remark" below.
- This protocol will result in subtherapeutic anticoagulation for 4-6 days.
- Plan 5: Hold warfarin only.
- Check INR 7 days before the procedure, keep INR in target range.
- Drop INR to 1.5 or less. For INR of 2.0-3.0, it will require about 4(3-5)days. Higher INR will take longer time.
- Check INR 1 day before the procedure. If INR is 1.8 or higher, give vitamin K 2.5 mg orally, or delay the procedure.
- Restart the previous maintenance dose of warfarin the evening of the procedure, If it cannot be started - see "Remark" below.
- This protocol will result in subtherapeutic anticoagulation for 6-8 days.
Subcutaneous unfractionated heparin or low dose low molecular weight heparin may be used for prevention of post operative venous thromboemboli.
For more urgent surgery, please review Section Managing High INR or Bleeding, "8. Patient who requires more rapid or urgent INR reversal before procedure/surgery".Large dose of intravenous Vit K may cause a period of warfarin resistance up to a week, when restart it.
Table 11. Low bleeding risks: Guidelines for managing anticoagulation during procedures/surgeries.
|
PROCEDURE/SURGERY |
BLEEDING RISK |
DIAGNOSIS |
THROMBO RISK |
PROTOCOL |
|
(Low bleeding risk) Others: |
. |
VTE/pulmonary emboli ** †† |
. |
. |
|
Low |
--- < 1 month |
High |
1, 2 |
|
|
Low |
--- 1-3 months |
High |
1, 2 |
|
|
Low |
--- Recurrent |
Low |
5, 1 |
|
|
. |
Acute Arterial Emboli †† |
. |
. |
|
|
Low |
--- < 1 month |
High |
1, 2 |
|
|
Low |
--- > 1 month |
Low |
5, 1 |
|
|
. |
Non Valvular atrial fibrillarion (NVAF) |
. |
. |
|
|
Low |
Atrial fibrillation |
Low |
5, 1 |
|
|
Low |
--- With risk factors (1) |
High |
1,2,3,4 |
|
|
. |
Heart Valve Prostheses |
. |
. |
|
|
Low |
Bileaflet AV † |
Low |
5, 1 |
|
|
Low |
Other valves, multiple or with additional risk factors (2) |
High |
1,2,3,4 |
|
| See "Thrombo embolic Risks" section |
Table 12. High bleeding risks: Guidelines for managing anticoagulation during procedures/surgeries.
|
PROCEDURE/SURGERY |
BLEEDING RISK |
DIAGNOSIS |
THROMBO RISK |
PROTOCOL |
|
(High bleeding risk) • Cutaneous: More complex procedures, i.e. hair transplantation, blepharoplasty, or facelifts.• Oral: More complex procedures such as complicated extractions, gingival and alveolar surgeries. • Opthalmic: Retinal surgery, complex lid and orbital surgery, patients who need retrobulbar anesthesia for ophthalmic procedures. • GI procedures: colonoscopic or gastric polypectomy, laser ablation and coagulation, endoscopic sphincterotomy, pneumatic or bougie dilation of strictures, percutaneous endoscopic gastrostomy, EUS-guided fine needle aspiration. • Cardiac procedures: Pacemaker/ICD insertion have more bleeding potential than bleeding from cardiac catheterization site. • Intracavitory surgery: Intraabdominal surgeries, intrathoracic surgeries, intracranial surgeries, • Neurosurgical procedures, neuraxial anesthesia and spinal puncture. • Orthopedic. • Genito-urinary: Transurethral resection of the prostate? • Obstetric-gynecologic. • plastic surgery. • Any procedures or surgeries that bleeding can not be controlled or stopped with simple intervention. Others: |
. |
VTE/pulmonary emboli ** †† |
. |
. |
|
High |
--- < 1 month |
High |
2 |
|
|
High |
--- 1-3 months |
High |
4, 2 |
|
|
High |
--- Recurrent |
Low |
5, 4 |
|
|
. |
Acute Arterial Emboli †† |
. |
. |
|
|
High |
--- < 1 month |
High |
2, 4 |
|
|
High |
--- > 1 month |
Low |
4, 5 |
|
|
. |
Non Valvular atrial fibrillarion (NVAF) |
. |
. |
|
|
High |
Atrial fibrillation |
Low |
5, 4 |
|
|
High |
---With risk factors (1) |
High |
4, 2 |
|
|
. |
Heart Valve Prostheses |
. |
. |
|
|
High |
Bileaflet AV † |
Low |
5, 4 |
|
|
High |
Other valves, multiple or with additional risk factors (2) |
High |
2, 4 |
|
Table 13 Simple guidelines for managing anticoagulation during procedures/surgeries.
Acute VTE
-- Month 1
-- Month 2-3
Recurrent VTE
Acute arterial embolism
-- Month 1
Mechanical heart valve
NVAF
- * = Hold Warfarin at apppropriate time (See "Detail of protocols for managing anticoagulation during procedures/surgeries, Table 10, 11, 12) or continue Warfarin if risk of bleeding is low. .
- ** = Start Warfarin at appropriate time if Warfarin is withheld. (See "Detail of protocols for managing anticoagulation during procedures/surgeries, Table 10, 11, 12)
- No detail in managing patients with different operative bleeding risk, or patients with different thromboembolic risk.
- VTE = Venous thromboembolism. NVAF = Non valvular atrial fibrillation.
- (2) = Unfractionated (UFH) or low molecular weight heparin (LMWH).
- (3) = For prevention of venous thromboembolism only.
Unfractionate heparin (UFH) (Update soon)
- Molecular weight of 3000 to 30000 and mean of 15000
LMWH (Low molecular weight heparin)
- Molecular weight of 2000 to 9000 and mean of 4000-5000.FDA has not approved for anticoagulation bridging therapy, but there has been sufficient data that it can be used effectively and safely.
- When compare to UFH, LMWH has better bioviability, more predictable dose responses and longer plasma half-lives. It has less interaction with platelets, endothelial cells. macrophages and plasma proteins, less heparin-induced thrombocytopenia (HIT) than UFH (1% vs 3%), and similar rate of bleeding to UFH.
- Can be given subcutaneously on an outpatient basis. It will require adequate plan and patient education to make it work properly
- Can be monitored with anti Xa level
- Antidote is protamine sulfate but only partially effective
- No effect on INR level.
Unsuitable conditions for LMWH:
Dosing
Prophylactic dose Therapeutic dose . . q 12 hours q 24 hours Enoxaparin 20-40 mg od 1 mg/kg 1.5 mg/kg Delparin 5000 IU od 100 IU/kg 200 IU/kg Nadroparin 38 IU od 87 IU/kg . Tinzaparin 4500 IU od 175 IU/kg . Before surgery dosing. Usually start 24-48 hours after last warfarin dose.
- Enoxaparin (Lovenox) 1mg/kg SC q 12 hours or 1.5 mg/kg SC q 24 hours.
- Dalteparin (Fragmin) 120 U/kg SC q 12 hours or 200 U/kg SC q 24 hours
- Tinzaparin (Innohep) 175 U/kg SC q 24 hours
After surgery dosing
- Therapeutic dose at no sooner than 24 hours after the procedure. Prophylactic dose may be started 12 hours after the procedure in not high bleeding risk patients.
- Continue heparin therapy until INR reaches therapeutic level for 2 consecutive days.
Heparin-induced thrombocytopenia (HIT)
- Incident of 3% from UFH and 1% from LMWH. May associate with thrombosis in 30-80% of the cases.
- May occur as early 1 day into therapy particularly in case with previous heparin exposure.
Table 15. Form for managing anticoagulation during procedures/surgeries.
Section A Section B Patient name: . Age: Rec No: . . 1ry Diagnosis: Thrombo risk: H, L* Bleeding risk: H, L* 2ry Diagnosis: Thrombo risk: H, L* Bleeding risk: H, L* Procedure/surgery: Thrombo risk: H, L* Bleeding risk: H, L* Select the protocol - Plan 1, 2, 3, 4, 5 (Circle the number) * H = high, Low = low.
(For more urgent surgery, please review Section Managing High INR or Bleeding, "8. Patient who requires more rapid or urgent reversal before procedure/surgery".)
1. Fill in the patient information in Section A. 1ry Diagnosis = Diagnosis that requires anticoagulation. 2ry Diagnosis = Diagnosis ( that may increase thromboembolic or bleeding risks.
2. Determine thromboembolic and bleeding risk in Section B. Then circle the H (high) or L (low). Using Table 9, Table 11, Table 12. for risk stratification.
3. Select the protocol plan. Using Table 11, Table 12, Table 10, and individualization for selection guidelines. Then circle the protocol plan number in Section C.
4. May print "Managing anticoagulation during procedures/surgeries section". M ay also mark those areas picked (underline or yellow mark). May send this marked printout to primary physician or place it in the chart.
Anticoagulation Guidelines for Endoscopic Procedures.
American Society for Gastrointestinal Endoscopy. Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures.
Gastrointest Endosc . 2002 Jun;55(7):775-9.
- Hold warfarin for 3-5 days
- Consider heparin while INR is sub therapeutic *- Hold warfarin for 3-5 day
- Re-institute warfarin right after the procedure- No change in anticoagulation
- Elective procedures should be delayed while INR is in supratherapeutic range* Use more detail guidelines for heparin bridging as described in the earlier section.
ASA and other NSAIDs: Endoscopic procedures may be performed in patients taking ASA or other NSAIDs if there is no pre-existing bleeding disorder.
Polypectomy Diagnostic: EGD +/- biopsy, flex sigmoidoscopy +/- biopsy, colonoscopy +/- biopsy
Billiary sphincterotomy ERCP without sphincterotomy Pneumatic or bougie dilatation Billiary/pancreatic stent without sphincterotomy PEG placement Endoscopy without fine needle aspiration Endosonic guided fine needle aspiration Endoscopy Laser ablation and coagulation Treatment of varices
Atrial fibrillation with valvular heart disease or prior thromboembolic event Deep vein thrombosis Mechanical valve in mitral position Uncomplicated or paroxysmal non-valvular atrial fibrillation Mechanical valve and prior thromboembolic event Bioprosthetic valve Very recent thromboembolic event or multiple and severe thromboembolic events Mechanical valve in aortic position
Options of anticoagulation management in pregnancy with mechanical prosthetic valve.
- Warfarin throughout pregnancy, with its potential fetal risks. Change to heparin (UFH or LMWH) at 38 weeks, Labor induction at 40 weeks of gestation.
- Heparin throughout pregnancy, with its associated maternal thrombosis risks particularly mechanical heart valve prosthesis. It is anticipated that heparin dose in the third trimester will be higher.
- Heparin during the first trimester. Switch to warfarin in the second trimester. Change back to heparin at 38 weeks. Labor induction at 40 weeks of gestation. Heparin dose in the third trimester is usually higher.
For UFH, start with total daily dose of 35000 U given subcutaneously twice a day. Monitor PTT at least twice a week to keep the level at least 2-3 times of control. For LMWH such as Lavenox, start with 100 mg given subcutaneously twice a day. Monitor anti-Xa to keep the level at 0.5 -1.2 U/ml 4-6 hours after injection.
Risk of mechanical heart valve prosthesis thrombosis in pregnancy continue to be high with heparin therapy. The heparin dose should be kept at high PTT or anti-Xa level.
General.
- Ginsberg JA, Crowther MA, White RH, Ortel TL. Anticoagulation Therapy. Hematology
Am Soc Hematol Educ Program) 2001 Jan; :339-57.- AHA/ACC. Foudation Guide to Warfarin Therapy, 2003
Circulation . 2003 Apr 1;107(12):1692-711. Review.- Ansell JE, Oertel LB, Wittkowsky AK. Managing Oral Anticoagulation Therapy. Clinical and Operational Guidelines. Lippincott Williams & Wilkins; 2 edition (June 1, 2005)
- Ansell JE, Buttaro ML, Thomas VO, et al. Consensus Guidelines for Coordinated Outpatient Oral Anticoagulation Therapy Management. Ann Pharmacother. 1997; 31: 604-615.
- ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation
Circulation. 2006;114:e257-e354.- ACC/AHA 2006 Guidelines for the Management of Patients with Valvular Heart Disease
Circulation . 2006 Aug 1;114(5):e84-231. Review.- Schulman S.
Clinical practice. Care of patients receiving long-term anticoagulant therapy.
N Engl J Med . 2003 Aug 14;349(7):675-83. Review.- Jack Ansell, M.D. Jack Hirsh, M.D. Nanette K. Wenger, M.D.
Postgraduate Education Committee, Council on Clinical Cardiology
American Heart Association
Warfarin Initiation.
- Crowther MA, Ginsberg JB, Kearon C, Hirsh J et al. A Randomized Trial Comparing 5 mg and 10 mg warfarin Loading Doses. Arch Intern Med, 1999; 159: 46-48.
- Tait RC, Sefcick A. A Warfarin Induction Regimen for Outpatient Anticoagulation in Patients with Atrial Fibrillation. Br J Haematol. 1998; 101(3): 450-454.
- Ageno W, Turpie AG. Exaggerated Initial Response to Wafrarin followint Heart Valve Replacement. Am J Cardiol, 1999; 84(8): 905-908.
- Kovacs MJ, Rodger M, Anderson DR, Morrow B, Kells G, Kovacs J, Boyle E, Wells PS.
Comparison of 10-mg and 5-mg warfarin initiation nomograms together with low-molecular-weight heparin for outpatient treatment of acute venous thromboembolism. A randomized, double-blind, controlled trial.
Ann Intern Med. 2003 May 6;138(9):714-9.Target INR.
- ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation
Circulation. 2006;114:e257-e354.- ACC/AHA 2006 Pocket Guidelines for the Management of Patients with Valvular Heart Disease
- Hylek EM, Go AS, Chang Y, Jensvold NG, Henault LE, Selby JV, Singer DE. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation.
N Engl J Med . 2003 Sep 11;349(11):1019-26.Warfarin Requirement for Pacific-Asian ( Exclude caucasian in this region)
- Dang MT, Hambleton J, Kayser SR. The influence of ethnicity on warfarin dosage requirement.
Ann Pharmacother . 2005 Jun;39(6):1008-12. Epub 2005 Apr 26.- El Rouby S, Mestres CA, LaDuca FM, Zucker ML.
Racial and ethnic differences in warfarin response.
J Heart Valve Dis . 2004 Jan;13(1):15-21. Review.Tatget INR for Pacific-Asian (Limited evidence-based)
- Yamaguchi T. Optimal intensity of warfarin therapy for secondary prevention of stroke in patients with nonvalvular atrial fibrillation : a multicenter, prospective, randomized trial. Japanese Nonvalvular Atrial Fibrillation-Embolism Secondary Prevention Cooperative Study Group.
Stroke . 2000 Apr;31(4):817-21.- Yasaka M , Minematsu K , Yamauchi T. Optimal intensity of international normalized ratio in warfarin therapy for secondary prevention of stroke in patients with non-valvular atrial fibrillation.
Intern Med 2001. Dec;40(12):1183-8.- Cheung CM, Tsoi TH, Huang CY. The lowest effective intensity of prophylactic anticoagulation for patients with atrial fibrillation.
Cerebrovasc Dis . 2005;20(2):114-9. Epub 2005 Jul 5.Vitamin K
- Crowther MA , Douketis JD , Schnurr T , Steidl L , Mera V , Ultori C , Venco , Ageno W . Oral vitamin K lowers the international normalized ratio more rapidly than subcutaneous vitamin K in the treatment of warfarin-associated coagulopathy. A randomized, controlled trial.
Ann Intern Med. 2002 Aug 20;137(4):I39.- Wilson SE , Watson HG , Crowther MA . Low-dose oral vitamin K therapy for the management of asymptomatic patients with elevated international normalized ratios: a brief review.
CMAJ 2004 Mar 2;170(5):821-4.- Gunther KE , Conwy G , Leibach L , Crowther MA . Low-dose oral vitamin K is safe and effective for outpatient management of patients with an INR>10.
Thromb Res. 2004;113(3-4):205-9- Dentali F, Crowther MA.
Management of excessive anticoagulant effect due to vitamin K antagonists.
Hematology Am Soc Hematol Educ Program. 2008:266-70.Perioperative Management.
- Kearon C. Perioperative Management of Long-term Anticoagulation. Semin Thromb Hemost 1998; 24 (Suppl 1): 77-83.
- Kearon C, Hirsh J. Managing Anticoagulation Before and After Surgery in Patients Who Require Oral Anticoagulants. N Engl J Med 1997; 336: 1506-1511.
- Heit JA. Perioperative management of the chronically anticoagulated patient.
J Thromb Thrombolysis. 2001 Sep;12(1):81-7. Review.- Wahl MJ. Dental Surgery in Anticoagulation Patients. Arch Intern Med, 1998; 158: 1610-1616.
- Randall C . Surgical management of the primary care dental patient on warfarin.
Dent Update. 2005 Sep;32(7):414-6, 419-20, 423-4 passim.- Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ 2nd, Waring JP, Fanelli RD, Wheeler-Harbough J; American Society for Gastrointestinal Endoscopy.
Guideline on the management of anticoagulation and antiplatelet therapy for endoscopic procedures.
Gastrointest Endosc . 2002 Jun;55(7):775-9.- Dunn AS, Turpie AG.
Perioperative management of patients receiving oral anticoagulants: a systematic review.
Arch Intern Med. 2003 Apr 28;163(8):901-8. Review.- Jaffer AK, Brotman DJ, Chukwumerije N.
When patients on warfarin need surgery.
Cleve Clin J Med. 2003 Nov;70(11):973-84. Review.- Dunn A . Perioperative management of oral anticoagulation: when and how to bridge.
J Thromb Thrombolysis. 2006 Feb;21(1):85-9.Warfarin Drug Interaction.
- Holbrook AM, Pereira JA, Labiris R, McDonald H, Douketis JD, Crowther M, Wells PS.
Systematic overview of warfarin and its drug and food interactions.
Arch Intern Med . 2005 May 23;165(10):1095-106. Review.- Wittkowsky AK, Boccuzzi SJ, Wogen J, Wygant G, Patel P, Hauch O.
Frequency of concurrent use of warfarin with potentially interacting drugs.
Pharmacotherapy . 2004 Dec;24(12):1668-74.- Greenblatt, D. J., von Moltke, L. L. (2005). Interaction of Warfarin With Drugs, Natural Substances, and Foods. J Clin Pharmacol 45: 127-132
Low Molecular Weight Heparin.
- Hirsh J, Warkentin TE, Shaughnessy SG, et al. Heparin and Low-Molecular-Weight Heparin: Mechanisms of Action, Pharmacokinetics, Dosing, Monitoring, Efficacy, and Safety. Chest 2001; 119 (Suppl 1): 64S-94S.
- Spandorfer j, Lynch S, Weitz HH, et al. Use of Enoxaparin for the Chronically Anticoagulated Patient Before and After Procedures. Am J Cardiol 1999; 84: 478-480, A10.
- Litin SC, Heit JA, Mees KA, et al. Concise Review for Primary-Care Physicians. Use of Low-Molecular-Weight Heparin in the Treatment of Venous Thromboembolic Desease: Answers to frequently asked questions. Mayo Clic Proc 1998; 73: 545-551.
Heparin Induced thrombocytopenia.
- Warkentin TE, Levine MN, Hirsh J, et al. Heparin-insuced Thrombocytopenia in Patients Treated with Low-Molecular-Weight heparin or Unfractionated Heparin. N Engl J Med, 1995; 332: 1330-1335.
- Magnani HN, Orgaran (danaparoid sodium) Use in the Syndrome of Heparin-induced Thrombocytopenia. Platelets 1997; 8: 74-81.
Anticoagulation During Pregnacy
- Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS; 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: Circulation. 2008;118:e523-e661
- Chan WS, Anand S, Ginsberg JS. Anticoagulation of pregnant women with mechanical heart valves: a systematic review of the literature. . Arch Intern Med. 2000;160:191-196.
- Geelani MA, Singh S, Verma A, Nagesh A, Betigeri V, Nigam M. Anticoagulation in Patients with Mechanical Valves During Pregnancy. . Asian Cardiovasc Thorac Ann 2005;13:30-33
Anticoagulation web sites
- www.acforum.org
Anticoagulation Forum.- www.coumadin.com
- Google Search for Oral Anticoagulation
- MSN search for Oral Anticoagulation
- Yahoo search for Oral Anticoagulation
- Google search for Anticoagulation Clinic Guidelines
- MSN search for Anticoagulation Clinic Guidelines
- Yahoo search for Anticoagulation Clinic Guidelines
Patient education and understanding is essential for successful warfarin management clinic.
- Keep content simple and uniform. It has been recommended that the 5th or 6th grade level is usually more effective.
- Include family member or significant other.
- Evaluate the patient understanding, cooperation and compliance periodically. Repeat education is usually necessary.
- It is a time consuming process and it is more effectively performed by specific personnel with experience and time.
Contents
- Why do they need anticoagulation.
- They have condition-disease with harmful blood clot or potentially harmful blood clot formation. The blood clot may block blood vessel such as in the leg or the lung. The more serious conditions are blood clot in the heart and in the blood vessel in the brain which can cause stroke.
- What is oral anticoagulation (Coumadin is a brand of Warfarin).
- It action is to help reduce the blood clot formation by decreasing the formation of blood clotting factors, not due to thinning of the blood as usually belief.
- Coumadin, Befarin, Orfarin, etc are brand names of Warfarin).
- Importance of compliance.
- What happen if the patient take too much or too little coumadin.
- Taking too much coumadin will cause bleeding.
- Taking too little coumadin will not prevent blood clot formation.
- Coumadin has narrow therapeutic range and it needs to be monitored carefully.
- How do we know that they take the right dose.
- Blood test to measure INR. There are INR levels that are recommended for various condition-diseases. Coumadin dose will be adjusted to obtain the appropriate INR level.
- Time to take coumadin and blood test.
- If it is possible, they should take coumadin in the afternoon-evening and have blood test in the morning. This will make the INR test result more consistent and enough time for the clinic to notify the patient the next doses of coumadin.
- Interactions.
- Medicine non compliance and drug interaction are the most common causes of fluctuating INR.
- Drugs:
- This includes both prescription drugs, over the counter medicines and herbal-natural products. The clinic should have adequate list of these products.
- Patient must report to the anticoagulation clinic or the health care provider as soon as they start on new medicine even it is a temporary one.
- The clinic should have plan or protocol to deal with drug interaction.
- Food:
- Recognizing food rich in vitamin K. The clinic should have list of those food for the patient.
- Patient should try to be on stable eating habit.
- Avoid alcohol.
- When to contact the clinic.
- New medicine or herbal remedies; concurrent illness; evidence of bleeding
- Patient must tell physician or dentist who will perform any procedures that they are taking oral anticoagulation.
- Medic alert bracelet or oral anticoagulation (warfarin) card
Dub Sukhum, MD.
Warfarin Tablet