 | |
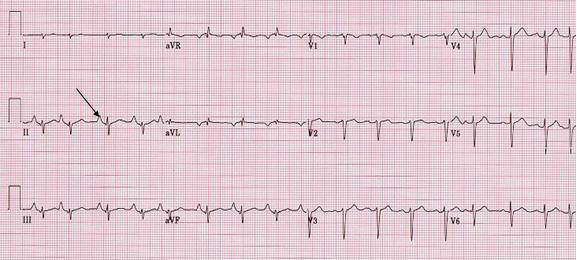
| II  V1 V1 | Comment. 1. V1 does not has criteria of RA abnormality. 2. There are few atrial premature depolarizations. 3. Other abnormality include ECG pattern consistent of severe lung disease patient. |
| RA abnormality | |
| P pulmonale is used when there is tall and peaked P wave in lead II, III and aVF, | |
| Patient. 80 year old male was admitted with acute exacerbation of his severe COPD. He also has history of coronary artery disease with non Q wave MI and 2 vessels stent placement in 5/02. Echocardiogram did not report of right heart enlargement and the pulmonary artery pressure was estimated to be only slightly elevated. Left atrial size was normal. There was left ventricular inferior wall motion abnormality with over all ejection fraction of about 55% | |
| P wave abnormalities. There are wide range of variation of P wave abnormalities since several factors may effect the P wave. These include: Anatomic cardiac position to the anterior chest wall; state of autonomic influence; intra and/or interatrial conduction abnormality; atrial pressure and/or volume load; atrial/atria diseases; electrode positioning (precordial lead). The diagnostic sensitivity are poor. | |
| LA abnormality, RA abnormality, or Intra/inter atrial conduction defect (IACD) are better term than LA enlargement or RA enlargement. | |
|
LA
abnormality | RA
abnormality |
|
• Prolonged P wave >120 ms (0.12 sec). • Notched P wave in lead II ( P mitrale). The 2 peaks should be apart >0.04 sec. • Terminal negative P wave in lead V1 area >0.04 (amplitude in mV x duration in second). • Left shift of P wave axis on frontal plane (from +45 and +60 to -30 and +45) | • Peaked
P wave in lead II (inferior leads) > 2.5 mV. • Initial positive P wave in lead V1 amplitude >1.5 mV and area >0.06 (amplitude in mV x duration in second). • Right shift of P wave axis on frontal plane (from +0 to +75 to more than + 75) |